Osteochondrosis is a chronic disease in which degenerative changes occur in the vertebrae and situated between them intervertebral disks. Depending on the lesion of the spine are: the cervical osteochondrosis, osteochondrosis of the thoracic and osteochondrosis of the lumbar spine. For the diagnosis of osteochondrosis of the spine need radiography, and in case of complications (eg, herniated disc) - spinal MRI. In the treatment of osteoarthritis of the spine along with the medical methods are widely used, reflexology, massage, manual therapy, physiotherapy and exercise therapy.
Etiology and pathogenesis
In varying degrees, osteochondrosis occurs in all aged people and is one of the aging process. Sooner or later in the intervertebral disc occur atrophic changes, however, of injury, disease, and the various overloads of the spine contribute to the earlier emergence of osteoarthritis. The most common osteochondrosis of the cervical and degenerative disc disease of the lumbar spine.
There are about 10 theories of degenerative disc disease: vascular, hormonal, mechanical, genetic, infectious-allergic and other. But none of them gives a complete explanation of what is happening in the spine changes, rather they are complementary.
It is believed that the main point in the occurrence of osteoarthritis is the constant overload of the vertebral motor segment, consisting of two adjacent vertebrae. This overload can result from movement patterns — posture, the individual manner of sitting and walking. Incorrect posture, sitting in a wrong posture, walking with an uneven spinal column cause extra strain on discs, ligaments and muscles of the spine. The process may be exacerbated because of the peculiarities of the structure of the spine and failure of trophic its tissues due to hereditary factors. Most often, the weaknesses in the structure occur in the cervical spine and lead to vascular disorders and early signs of degenerative disc disease of the cervical spine.
The occurrence of osteochondrosis of the lumbar often associated with his overload when bending and lifting weights. A healthy intervertebral disc can withstand considerable loads due to the hydrophilicity located in the center of nucleus pulposus. The kernel contains a large amount of water and fluid, as you know, a little compressed. Rupture of a healthy intervertebral disc can occur when the force of compression of more than 500 kg, while changed as a result of degenerative disc disease the disc is broken when the force of compression of 200 kg. Load 200 kg experiences a lumbar spine of a person weighing 70 kg, when he holds a 15-pound load in the position of the torso forward at 200. Such a large pressure due to the small size of the nucleus pulposus. When the inclination increases to 700, the load on the intervertebral discs is 489 kg. So often the first clinical manifestation of osteochondrosis of the lumbar spine occur during or after heavy lifting, performing household chores, weeding the garden, etc.
The destruction of the connective tissue of the fibrous ring of the disc, ligaments and capsules of the facet joints causes a reaction of the immune system and the development of aseptic inflammation with swelling of the facet joints and surrounding tissues. Due to the displacement of the vertebral body is stretching of the capsule of the facet joints, and changed the intervertebral disc is not so firmly locks the body of the adjacent vertebrae. Formed the instability of the spinal segment. Due to the instability of possible infringement of the nerve root of the spinal nerve with the development of radicular syndrome. Osteochondrosis of the cervical spine frequently occurs during cornering of the head, osteochondrosis of the lumbar spine during trunk bending. The formation of the functional unit of the vertebral motor segment. It is due to the compensatory contraction of the muscles of vertebrates.
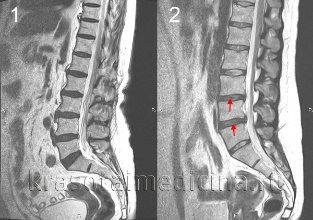
A herniated disc occurs when the disc moves backwards, there is a rupture of posterior longitudinal ligament and bulging of the disc into the spinal canal. If the spinal canal is squeezed out the nucleus of the disk, this is called a ruptured hernia. The severity and duration of pain associated with a hernia is much more than the unexploded. A herniated disc may cause radicular syndrome or spinal cord compression.
When osteochondrosis occurs, the expansion of the bone with formation of osteophytes — bony growths on the bodies and vertebrae. Osteophytes can also cause compression of the spinal cord or cause the development of radicular syndrome.
The symptoms of osteochondrosis
The main symptom of osteochondrosis is pain. The pain may be sharp with high intensity, it increases with the slightest movement in the affected segment and, therefore, forces the patient to take a forced situation. So in osteochondrosis of the cervical spine, the patient keeps the head in the least painful position, and cannot rotate, osteochondrosis of the thoracic the pain is worse even with a deep breath, and osteochondrosis of the lumbar the patient is difficult to sit, stand and walk. Such a pain syndrome is characteristic of compression of the nerve root of the spinal nerve.
Approximately 80% of cases, there is dull pain constant in nature and of moderate intensity. In such cases, during the examination the doctor needs to differentiate manifestations of osteochondrosis of the spine from myositis of the back muscles. Dull pain in osteochondrosis is caused by the excess voltage of the muscles that hold the affected vertebral motor segment, inflammatory changes or significant stretching of the intervertebral disc. Patients with this pain syndrome forced position is missing, but revealed limitation of movement and physical activity. Patients with osteochondrosis of the cervical spine, avoid sharp turns and tilts her head, osteochondrosis of the lumbar - slowly sit up and get up, avoid trunk bending.
Complications of spinal osteochondrosis
Complications of degenerative disc disease associated with disc hernia. These include spinal cord compression, which is characterized by numbness, weakness of certain muscle groups of the limbs (depending on the compression level), leading to the appearance of the paresis, muscular atrophy, changes of tendon reflexes, disturbances of urination and defecation. Intervertebral hernia can cause compression of the artery feeding the spinal cord, with the formation of ischemic areas (infarction of the spinal cord) with loss of nerve cells. This is manifested by the appearance of neurological deficit (violation of movements, loss of sensitivity, trophic disorders), appropriate level and distribution of ischemia.
Diagnosis of osteochondrosis
The diagnosis of osteochondrosis is conducted by the neurologist or spine. At the initial stage produce x-rays of the spine in 2 projections. If necessary, you can make a survey of individual vertebral segment and shoot additional images. For the diagnosis of intervertebral hernia, assessment of the spinal cord and to detect complications of degenerative disc disease used magnetic resonance imaging (MRI of spine). Large role played by MRI in the differential diagnosis of osteochondrosis and other diseases of the spine: tuberculous spondylitis, osteomyelitis, tumors, ankylosing spondylitis, rheumatism, infections. Sometimes in complicated cases of degenerative disc disease of the cervical spine exclusion is required syringomyelia. In some cases, at impossibility of MRI myelography is shown.
Sighting study the affected intervertebral disc is possible with discography. Electrophysiological studies are used to determine the extent and localization of lesions of the nervous pathways, and the monitoring of their recovery during therapy.
Treatment of osteochondrosis
In the acute period are shown at rest in the affected vertebral motor segment. With this goal in osteochondrosis of the cervical spine is used, the fixation by means of collar Trench, osteochondrosis of the lumbar in bed. Fixation is required and in osteochondrosis of the cervical instability of the spinal segment.
In drug therapy for degenerative disc disease use of nonsteroidal anti-inflammatory drugs (NSAIDs): diclofenac, nimesulide, lornoxicam, meloxicam. With intense pain syndrome shows analgesics, for example, the Central analgesic action flupirtine. To relieve muscle tension and use muscle relaxants — tolperisone, tizanidine. In some cases, the appropriate use of anticonvulsants carbamazepine, gabapentin; antidepressants, among which preference is given to inhibitors of serotonin reuptake (sertraline, paroxetine).
Upon the occurrence of radicular syndrome patient shown inpatient treatment. Perhaps a local injection of glucocorticoids, treatment against edema, the use of traction. In the treatment of osteoarthritis are widely used physiotherapy, reflexology, massage, physiotherapy. The use of manual therapy requires strict adherence to techniques of execution and special caution in the treatment of degenerative disc disease of the cervical spine.
Surgery shown primarily with significant spinal cord compression. It consists of removing the herniated disc and decompression of the spinal canal. It is possible to conduct microdiscectomy and laser disc reconstruction, replacement of the affected disc implant, and the stabilization of the spinal segment.












































